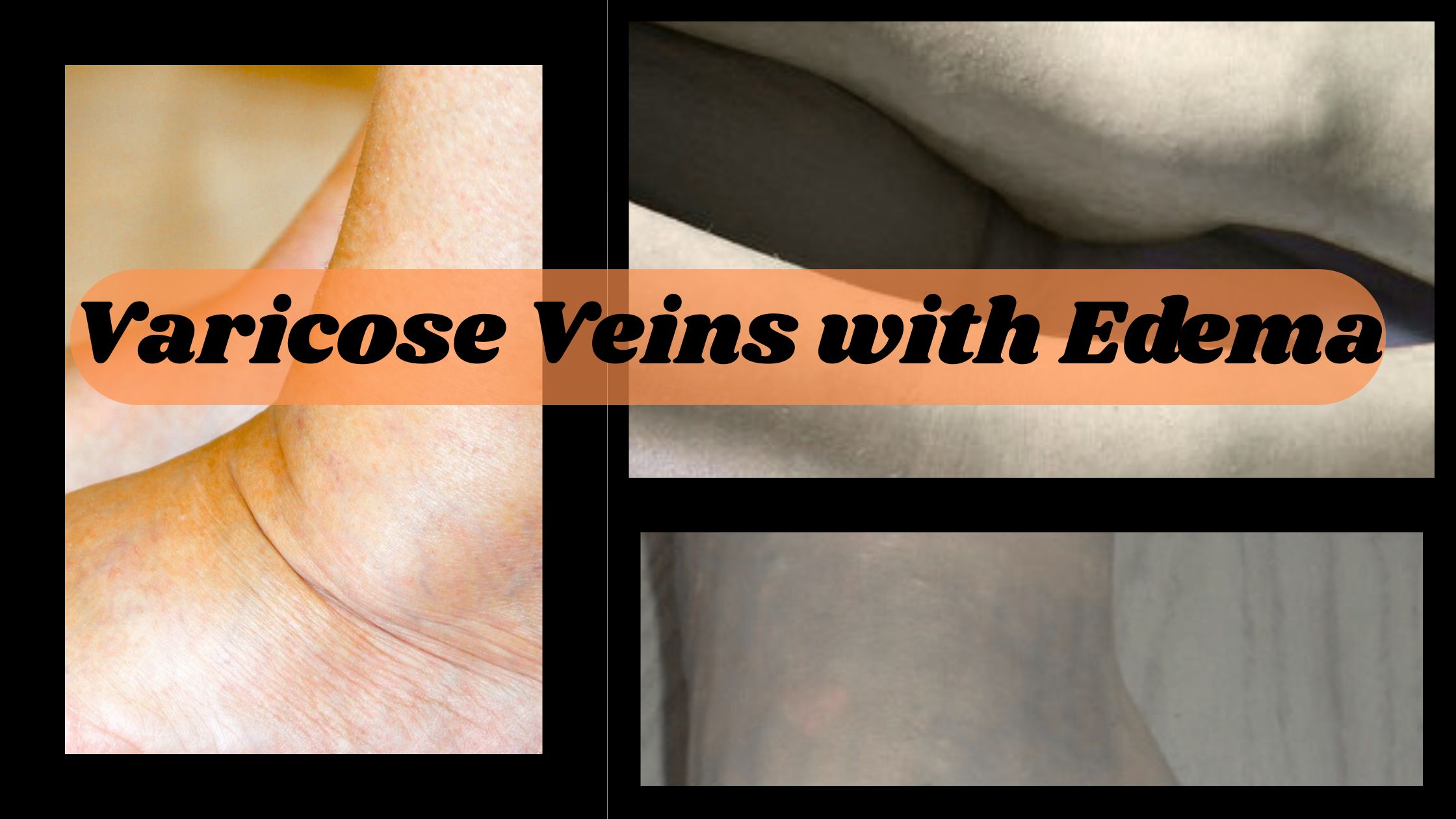
Varicose veins with edema represent a common yet often misunderstood vascular condition that affects millions of people worldwide. Characterized by twisted, enlarged veins and swelling in the affected areas, this condition can lead to discomfort, cosmetic concerns, and, in some cases, serious health complications. This article explores the nature of varicose veins with edema, their causes, symptoms, treatment options, and the distinction between nerve pain vs vascular pain, providing a comprehensive guide for those seeking to understand or manage this condition.
What Are Varicose Veins?
Varicose veins are enlarged, gnarled veins that typically appear in the legs and feet. They occur when veins become stretched and weakened, causing blood to pool rather than flow efficiently back to the heart. This pooling results from faulty valves within the veins, which normally prevent backward blood flow. When these valves fail, blood accumulates, leading to the bulging, rope-like appearance of varicose veins. While varicose veins are often seen as a cosmetic issue, they can cause significant discomfort and lead to complications, including edema.
Understanding Edema in the Context of Varicose Veins
Edema occurs when the impaired blood flow in varicose veins increases pressure in the veins, forcing fluid into surrounding tissues. This fluid buildup causes swelling, which can range from mild to severe. In the context of varicose veins, edema is often a sign of chronic venous insufficiency (CVI), a condition where the veins struggle to return blood to the heart effectively.
Symptoms of varicose veins with edema include:
- Visible, twisted veins under the skin, swelling in the legs, ankles or feet
- Pain, heaviness or throbbing sensations in the legs
- Itching or burning around affected veins
- Change (discoloration) or thicken the skin near the veins
- Muscle cramps or restless legs
Left untreated, varicose veins with edema can lead to complications such as skin ulcers, infections, or blood clots, making early intervention crucial.
Causes and Risk Factors
Several factors contribute to the development of varicose veins and associated edema. These include:
- A family history of varicose veins increases the chances of developing the condition.
- As we age, veins lose elasticity and valves weaken, contributing to blood pooling.
- Varicose veins are more likely to develop in women due to hormonal changes during pregnancy, menopause or contraceptive pills use.
- Jobs or lifestyles that include prolonged sedentary can disrupt blood flow.
- Overweight puts extra pressure on the veins, which increases venous insufficiency.
- Increasing blood volume and pressure from the growing uterus can lead to varicose veins and edema.
- Lack of physical activity makes those muscles weaker which help pump blood through the veins.
Understanding these risk factors can help individuals take preventive measures to reduce the chances or severity of varicose veins and edema.
Nerve Pain vs Vascular Pain: Understanding the Difference
An important aspect of managing varicose veins with edema is to differentiate between nerve pain vs vascular pain, as both can have similar symptoms, but different methods are needed for treatment.
Nerve Pain
Nerve pain, or neuropathic pain, arising from damage or dysfunction in the nervous system. It is often described as irritation, tingling or shooting sensations, sometimes with sensitivity to numbness or touch. In terms of varicose veins, nerve pain can occur when swollen tissues compress the nearby veins or if complications like venous ulcers irritate nerve endings. Conditions like peripheral neuropathy or sciatica can also mimic varicose veins symptoms, making the exact diagnosis necessary.
Vascular Pain
Vascular pain, on the other hand, is caused by problems within blood vessels, such as inflammation, poor circulation, or blood clots. In varicose veins with edema, vascular pain usually feels like heaviness, pain or throbbing in the legs, which often worsens after standing/sitting for a long time. The pain is directly related to the blood deposit and increased pressure in the veins, which can also contribute to inflammation and restlessness.
Differentiating the Two
Distinguishing between nerve pain and vascular pain is critical for effective treatment. Vascular pain associated with varicose veins often improves with elevation of the legs, compression therapy, or movement, as these actions promote blood flow. Nerve pain, however, may not respond to these measures and may require neurological evaluation or specific medications like gabapentin. Consulting a healthcare provider for a thorough assessment, including imaging or nerve conduction studies, can help clarify the source of pain.
Diagnosis and Evaluation
Diagnosing varicose veins with edema usually includes a review of physical exam and medical history. A healthcare provider can assess the veins appearance, check swelling and inquire about symptoms such as pain or heaviness. Diagnostic tools such as Doppler ultrasound can evaluate the blood flow and identify the valve’s dysfunction or blood clots. In cases where nerve pain is suspected, additional tests like electromyography (EMG) can be used to assess nerve function.
Treatment Options for Varicose Veins with Edema
Varicose veins managing with edema focuses on relieving symptoms, improving blood circulation and preventing complications. Treatment options depending on the severity of the condition range from conservative measures to medical intervention.
Conservative Treatments
- Wearing CS (compression stockings) helping improve blood flow, reduce inflammation and alleviate discomfort. These clothes put light pressure on the legs, which helps the functioning of the veins.
- Exercise (daily), weight management and avoiding prolonged sitting/standing can prevent worsening of symptoms.
- Leg elevation above heart level for 15–30 minutes several times a day can reduce edema and improve circulation.
- Staying hydrated and taking a balanced diet with low sodium can help manage fluid retention and inflammation.
Medical and Surgical Interventions
- A minimally invasive procedure in which a solution is injected into affected veins, from which they shrink and fade (Sclerotherapy).
- Laser or RFA uses energy to close problematic veins, giving blood flow redirected towards healthy veins (Endovenous Ablation).
- A surgical process of removing severely affected veins that are usually reserved for advanced cases (Vein Stripping).
- In cases where nerve pain exists, medications such as anti-inflammatory or nerve-specific drugs can be prescribed (Medications).
Managing Nerve Pain vs Vascular Pain
For vascular pain, treatment such as compression therapy and ablation is effective in addressing the underlying venous issues. For nerve pain, additional intervention such as physical therapy, nerve blocks or medications may be necessary. For those patients, vascular experts and neurologists may require multi -disciplinary approaches that experience both types of pain.
Prevention Strategies
To prevent varicose veins and edema it is necessary to adopt habits that promote healthy circulation:
- Consistent physical activity, like walking or swimming, which help to strengthen leg muscles and improve blood flow.
- Maintain healthy weight to reduce pressure on the veins.
- Avoid wearing tight clothes that disrupt blood flow.
- If your work involves sitting/standing for a long time, take a break every hour.
- Wear compression stockings while long flights or sitting.
When to Seek Medical Attention
Although light varicose veins and edema can often be managed at home, there are some symptoms that require immediate medical attention:
- Sudden or severe swelling in the legs
- Frequency of pain or heat in the affected area(could be sign of blood clot)
- Changes in skin, such as ulcers or open wounds
- Symptoms of nerve pain, like tingling or numbness, which do not improve with conservative measures
Living with Varicose Veins and Edema
Varicose veins with edema can affect the quality of life, causing physical discomfort and emotional distress due to cosmetic concerns. However, with proper management, most individuals can lead active, healthy lives. Understanding the difference between nerve pain vs vascular pain is an important step in preparing treatment according to the needs of a person. By combining lifestyle changes, medical intervention and regular follow-up with healthcare providers, patients can effectively manage symptoms and reduce the risk of complications.
Conclusion
A varicose vein with edema is a healing condition for which there are many management options. Whether conservative measures such as compression therapy or through advanced processes such as sclerotherapy, individuals can get relief and improve their vascular health. If you suspect that you have a varicose veins or are experiencing symptoms of edema or pain, consult a healthcare professional for a personal treatment plan.