- admin
- 0 Comments
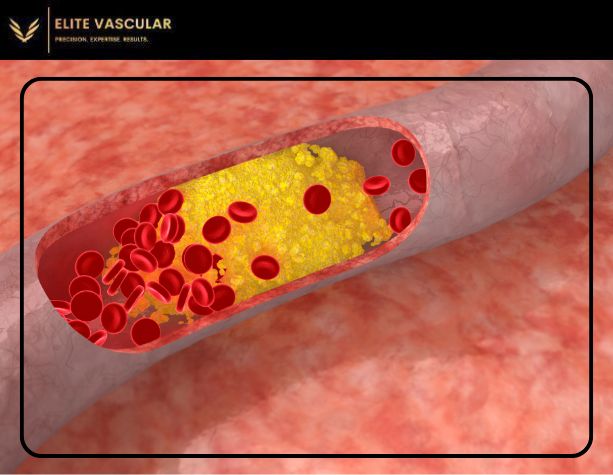
Peripheral Artery Disease (PAD) is defined as a common circulatory problem in which the arteries become narrowed and thus less blood is sent to the extremities, especially the legs. This is primarily due to atherosclerosis, which is plaque deposition along the arterial walls that deprives the muscles of the required blood. PAD is usually associated with the incapacity to walk without leg pain; nevertheless, the disease can develop into even more dangerous consequences if untreated.
It is important to know about the disease PAD including the symptoms and what methods are available in order to manage the disease and the vascular health of the patient. This section will define what PAD is and how it is possible to treat it.
What are the Symptoms of PAD?
There are relatively few primary symptoms and they tend to be rather mild or other times infrequent with the onset of the disease, making early diagnosis of the disease a difficult task. As the condition progresses however, clear symptoms make their presence felt. The most common manifestations of PAD are as follows:
Claudication (Leg Pain While Walking)
Among the many claudication symptoms, Leg Pain when walking or moving may be one of the first to be experienced by the patient suffering from Peripheral Artery Disease. It is an aching/cramping pain that disappears until the muscles are worked upon like when climbing the stairs or walking over a certain distance. Claudication often improves with rest. However, after a period of time and once the patient resumes upon physical activity again, the pain returns.
Weakness of the Leg
Lack of blood flow can result in leg numbness or leg weakness especially within individuals with PAD.
Coldness to the Lower Leg Area
Due to poor blood flow, the affected areas are likely to be cooler than the rest of the body.
Slow Healing of Wounds
In serious instances, it is possible that there is a painless foot ulcer or a sore on the leg, that, due to the limited blood circulation, will take an excessive amount of time to heal or remain in that state forever.
Skin Texture Changes Eg Rosiness Of Shins
The surface of the skin in calves and feet turns shiny or white or has a hue of blue or blue grey due to the low blood perfusion.
No or Less Growth Of Hair On The Legs And Feet
Chances of having hair on the legs and feet are minimal since the blood supply is in constant recession, hence hair is either scanty or grows at a slow rate.
All these symptoms, more so the claudication symptoms are aggravating factors which should send someone to see a health care practitioner. Because amputation is the last option to take when it comes to patients suffering from PAD, timely diagnosis and treatment should be maximized to prevent other related complications including particularly non healing wounds, infections etc.
Factors That Would Put One at Risk for PAD
There are many risk factors that are associated with the development of PAD. They include:
Smoking
This is among the worst risk factors of developing PAD. It leads to the destruction of blood vessels and speeds up the formation of plaques on the walls of arteries.
Diabetes
This condition puts one at high risk of developing PAD since high glucose levels are known to cause the damage of blood vessels resulting in poor blood flow.
High Blood Pressure
The excessive pressure exerted by blood on the arteries causes damage to the vascular structure making them susceptible to further damage and atherosclerosis.
High Cholesterol
High cholesterol levels in the blood lead to deposits of cholesterol plaque which serves to obstruct the arteries.
Obesity
Excess weight adds an excessive burden to the heart therefore extends the working capability of the atherosclerotic process.
Age
With increase in age the chances of getting PAD also increases especially when one is over the age of 50.
Family History
If one has a close relative, whose medical history includes heart diseases, strokes, or PAD, the same would apply to an individual at risk to go through this disease.
What Diagnostic Tests are Used to Identify PAD?
When a healthcare provider comes across a patient with PAD; there are several tests subdivisions that generally should seek to corroborate the typical diagnosis:
Ankle-Brachial index (ABI)
In this painless examination, the pressure in the dilemmas of the limbs is compared with the delimitation in the upper limb. Discrepancy in pressure values indicates that the blood vessels of the lower legs are fully or partially obstructed.
Ultrasound
The Doppler ultrasound scans are utilized in tracking the blood flow in the regions of the right arteries to diagnose any blood clot.
Angiography
Despite any invasive measures what may be resorted to is the introduction of the contrast in examination area and capturing the appropriate images to picture the certain arteries and determine the extent of their narrowing or even blockage.
Blood Tests
One of the approaches will be blood testing in order to assess other common risks, for instance cholesterol levels and diabetes, factors which could contribute to the high prevalence and incidence of PAD.
Management of PAD
The primary aim of the management of PAD is to bring back perfusion in the areas affected reduce the signs and avert the likelihood of such events occurring. Treatment methods include change of lifestyle, medication, and surgical methods where deemed necessary.
Lifestyle Modifications
Lifestyle changes are always and continue to be the best first-line therapy in management of PAD. Such modifications should include:
- Quitting Smoking: Whenever there is further exposure to smoking, it is hard to regain any further protection against injury to the blood vessels due to the interference from smoking tobacco.
- Exercise: Regular physical activity, such as walking, can improve circulation and relieve ailments associated with claudication.
- Healthy Diet: Following a heart-healthy diet with low saturated fats, cholesterol, and salt is effective in controlling cholesterol levels and blood pressure hence reducing the occurrence of plaque formation
- Weight Management: Doing some exercises to maintain a healthy body helps relieve the circulatory system from excess pressure and stress.
Medications
Most patients with PAD will be treated with medications, especially:
- Antiplatelet Drugs: Widespread use of antiplatelet therapy to prevent further vascular events in patients with a high thromboembolic risk.
- Cholesterol-Lowering Drugs: Statin cholesterol therapy has been associated with significant regression of atherosclerotic plaques and improved blood flow.
- Blood Pressure Medications: Effective control of hypertension helps to relieve stress from the arteries and diminish the risk of additional injury.
Surgical Procedures
If PAD is severe and medications do not help enough to relieve the pain, tissue or vascular surgery may be performed to reroute blood to improve PAD. Typical methods of intervention are:
- Angioplasty: The passage through the narrowed artery is enlarged by inserting and inflating a small balloon, a stent is sometimes placed to prevent the artery from collapsing.
- Bypass Surgery: In this approach, it creates a backward movement around the blocked artery using a blood round from other body parts, which helps restore blood supply to the limb.
Supervised Exercise Programs
Supervised exercise programs, which are also known as exercise therapy, enable a person to achieve a certain degree of walking function and decrease further complaints. Such programs are usually managed by specialists who demonstrate exercises to patients with the aim of enhancing blood flow.
Preventing PAD: Proactive Measures
Given that the occurrence of particular PAD risk factors like old age or family history is unpreventable, there are measures that can be undertaken in advance with an intention of hindering the occurrence of the disease.
- Live a Healthy Lifestyle: Incorporation on information stands that eating healthy, exercising and observing the body weight will assist in the prevention of PAD.
- Set Blood Sugar levels: People with diabetes ought to standardize their blood sugar levels or fox ensure their vessels are in good health.
- Cholesterol and Blood Pressure Control: Such things reduce these risk factors when done on regular basing.
- No Smoking: For smokers, the most critical thing that would help reduce the risk for PAD as well as for other vascular diseases is cessation of the habit.
Wrap-Up on PAD
In summary, Peripheral Artery Disease (PAD) is a very serious ailment and if not treated it can be quite dangerous. Nonetheless, through early diagnosis and the right intervention, it is possible to slow the development of PAD, reduce the signs that have already appeared, and prevent further complications. These individuals are capable of enhancing their quality of life and maintaining better vascular health by making personal lifestyle adjustments, using medications as indicated, and in some cases, undergoing surgical intervention. If this older population has any symptoms of or risk factors for PAD, they need to see a doctor for an appropriate diagnosis and management plan.